When it comes to barrier braindeath, the concept of a “6-12 minute barrier” plays a significant role in determining whether brain death can be declared. Brain death refers to the complete and irreversible cessation of all brain activity, including the brainstem, which controls vital functions such as breathing, heart rate, and reflexes. If the brain is deprived of oxygen for more than a brief period, such as through a traumatic injury or lack of blood flow, irreversible damage can occur, leading to brain death. But how does this 6-12 minute window factor into the process, and what does it mean for the diagnosis of brain death?
What is barrier brain Death?
Before understanding the 6-12 minute barrier, it’s essential to first grasp what brain death entails. Brain death occurs when the brain ceases all functions, including those of the brainstem, and cannot recover. It differs from conditions like a coma or vegetative state because, in brain death, there is no possibility of recovery. Brain death is considered legally and clinically equivalent to death.
Typically, brain death results from traumatic injuries (such as severe head trauma), anoxic brain injuries (caused by a lack of oxygen), or massive strokes. When the brain is deprived of oxygen, its cells begin to die, and irreversible damage occurs. Without oxygen, the brain cannot function, and within minutes, the damage becomes catastrophic.
The 6-12 Minute Barrier: A Critical Timeframe
The 6-12 minute barrier refers to the critical period after the brain loses its blood and oxygen supply. If the brain is deprived of oxygen for longer than 6 minutes, irreversible brain damage is likely to occur. This time period is often cited by doctors and neurologists as a guideline for when brain death becomes inevitable. However, the exact time frame can vary depending on the individual’s health and the specific circumstances of the injury.
Research has shown that the brain is extremely sensitive to a lack of oxygen. After 4 minutes without oxygen, brain cells begin to die, and after 6 minutes, the damage becomes severe. By the 10-minute mark, irreversible brain death is almost certain. This is why medical professionals are highly focused on the time elapsed since a traumatic event, especially in cases where a person is resuscitated after cardiac arrest or severe trauma.
The Role of the Brainstem and Apnea Test
The brainstem is a critical part of the brain responsible for autonomic functions like breathing, heart rate, and blood pressure regulation. When brain death is suspected, a series of neurological tests are performed to assess brain function. One key test is the apnea test, where the patient is taken off ventilator support to see if they will initiate breathing on their own. If there is no respiratory effort, it is a sign that the brainstem has completely failed.
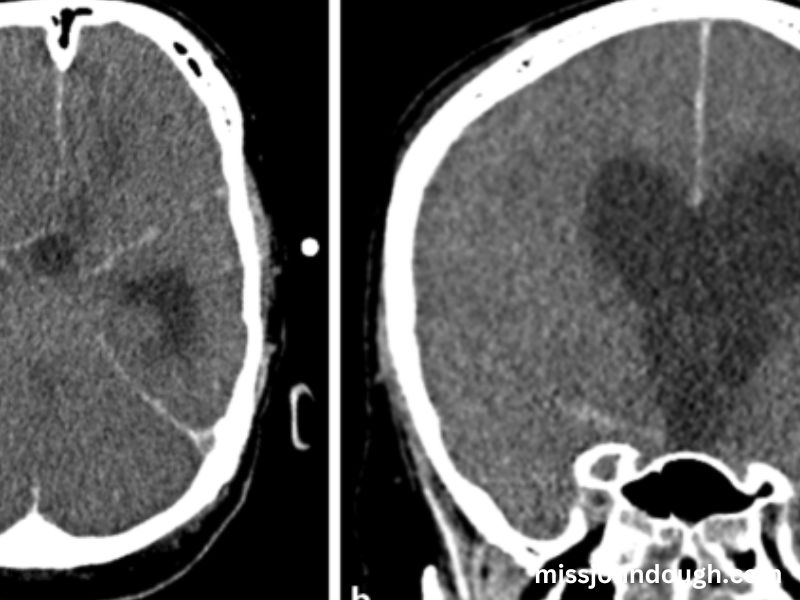
The apnea test, combined with other diagnostic procedures like neurological examinations and imaging tests (e.g., CT scans or MRIs), helps doctors confirm brain death. If the test results show no activity in the brainstem, and the patient fails to breathe independently, the diagnosis of brain death can be made.
Determining Brain Death in Different Conditions
While the 6-12 minute window is a general guideline, the actual time for brain death can vary depending on several factors. These include the person’s age, the severity of the injury, their overall health, and whether there are any conditions that might prolong the brain’s function. For instance, in cases of hypothermia, where body temperature drops significantly, the brain may be able to survive longer without oxygen due to reduced metabolic demands. In such cases, doctors may wait longer before diagnosing brain death.
Other conditions, such as drug overdose or intoxication with substances like barbiturates or narcotics, can mimic the symptoms of brain death. In such instances, doctors must be absolutely certain that the brain’s functions are not impaired due to external factors before declaring brain death.
The Legal and Ethical Considerations
The process of diagnosing brain death involves strict legal and ethical considerations. Once brain death is confirmed, the person is legally dead, and they are no longer considered to be alive. In many places, organ donation may be discussed, as individuals who are brain dead but still maintain circulation (due to mechanical ventilation) may be potential organ donors.
However, the declaration of brain death can be a sensitive and challenging issue for families, especially if they have not fully grasped the concept of brain death. Medical professionals must take great care to explain the situation and provide the family with support and counseling.
The Aftermath of Brain Death Diagnosis
Once brain death is diagnosed, the next steps depend on the family’s wishes and legal considerations. In many cases, the person will be kept on a ventilator to maintain organ function until family members decide whether to donate organs. The ventilator is not keeping the person alive; instead, it preserves vital organs for potential donation. Organ donation is a significant medical and ethical decision that requires clear communication with the family.
Can Brain Death Be Reversed?
Once brain death has occurred, it is irreversible. Unlike other medical conditions, there is no chance of recovery. Brain death signifies the end of brain activity, and no medical intervention can bring the brain back to life. This is why the 6-12 minute window is so critical—if the brain does not receive oxygen within this time frame, recovery becomes impossible.
Conclusion: The Importance of Timing in Diagnosing Brain Death
The 6-12 minute barrier highlights the importance of early medical intervention following severe trauma or cardiac arrest. While the exact timeframe for brain death can vary, the general consensus is that if oxygen is cut off from the brain for more than six minutes, irreversible damage will occur. Healthcare professionals use this window of time to perform diagnostic tests and determine whether brain death has occurred. Understanding the significance of this period can help families, doctors, and caregivers navigate the complex and often emotional process of brain death diagnosis and decision-making.
In the realm of medical ethics and legalities, the confirmation of brain death is a definitive event, marking the irreversible end of life. It is a stark reminder of the importance of prompt and effective care for individuals suffering from traumatic injuries or medical crises to prevent permanent damage to the brain.